What exactly are “Shin Splints”?
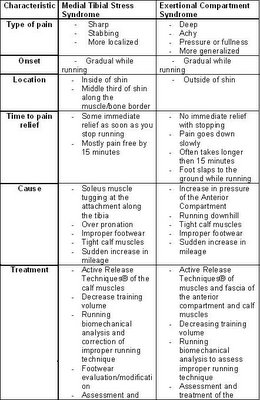
The term “shin splints” is a common diagnosis given when someone is suffering from pain in the front of their legs and is often associated with running. There are two main types of shin splints. They both have very similar symptoms but are significantly different in their actual diagnosis and treatment. So how can you tell them apart? Let's start with a description of both and then compare them…
FIRST TYPE
Medial Tibial Stress Syndrome (MTSS), as the name describes, is caused by pain along the medial (inside) part of the tibia (shin bone). The pain typically develops over a steady time while running and can be painful enough to make you want to stop. The pain is sharp and it decreases significantly once you stop running and after about 15 minutes is almost completely gone. You will also find that your shins are tender or painful to the touch along the middle third of the inside of the tibia. This type of shin splint usually begins with the onset of a new running activity and/or a sudden or rapid increase in mileage. An increase in body weight and running on hard surfaces has also been known to lead to this type of shin pain.
So what causes this pain? It is caused by the Soleus Muscle that attaches to the tibia along its inside border.
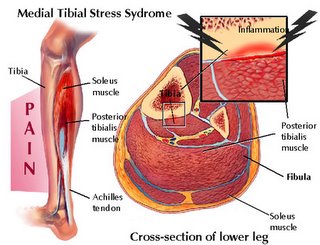
This muscle lies deep to the Gastrocnemius (bigger, bulkier muscle on the back of the leg) and together they form the “calf muscles”. The Soleus is composed of slow twitch muscle fibers, which means it is involved in endurance activities such as running, walking and even maintaining your standing posture. Once this muscle gets tight and/or overworked from sudden increases in running mileage or when starting a new activity, the muscle begins to tug at the attachment along the medial border of the tibia. This is what ends up causing the pain on the inside of the shin. The body naturally wants to try to stop the painful tugging, so it lays down scar tissue along the attachment to help reinforce it. However this only causes the muscle to become more tight and places even more stress along the attachment at the shin. This creates a viscious cycle of pain and tightening that will continue either until you get treatment, stop the activity, or modify the activity to provide enough time for proper healing.
SECOND TYPE
The second type of shin splints is also associated with a sudden increase in running mileage, and/or the beginning of a new running activity. The pain in with this type of shin splint is often worse running down hill, the pain is a deeper, achy pain and can lead to a slapping foot while running. Once you stop running the pain does not go away immediately and can still be very painful at rest 15 minutes after stopping. This time the pain is lateral (on the outside) of the tibia and is often described as a fullness or pressure feeling in the leg and is called an Exertional Compartment Syndrome.
The cause of the pain in this scenario is an increase in pressure in the anterior compartment of the leg. This compartment is formed between the tibia and fibula (the two bones in the lower leg) and a thick layer of fascia around the front. In this compartment lies the Tibialis Anterior muscle as well as the muscles that extend your toes. When you are running, these muscles help to lift (dorsiflex) your foot and toes to allow ground clearance while in the swing phase of running. They also help to slowly lower your foot and toes to the ground after heel strike at the beginning of the stance phase of running. When you contract a muscle, there is an increased need for blood to supply enough nutrients to keep it working. This increased blood supply to the muscle in turn increases the size of the muscle. This process is normal and usually goes unnoticed, however if the size or volume of the muscle increases too much, especially when the muscle is held tight like in the anterior compartment, it results in an increase in pressure and this causes pain. The pressure in the anterior compartment can get high enough that it affects the muscles ability to work, and this is why you may experience your foot slapping the ground while running. This results because the muscles can no longer lower your foot and toes slowly to the ground once you have heel contact so they just slap down uncontrollably. If the pressure continues to go up, it can even shut off the sensory nerve contribution to the skin between your first two toes.
Treatment Options
In order to decrease the pain associated with MTSS, the amount of pulling that the Soleus muscle exerts on the tibia must be decreased. This can be accomplished in several ways. The first is by treating the Soleus with muscle soft tissue techniques such as ART® and Graston. These techniques have been developed to help break up scar tissue, release adhesions between muscles and restore normal muscle tone. By using these techniques, the tension on the tibial attachment of the Soleus is lowered thereby decreasing the pain at that area. More treatment options include walking/running biomechanical analysis. Performed properly, this can reveal functional mechanics that may be predisposing to MTSS. Some predisposing factors include overpronation, rearfoot varus deformity and leg length discrepancy. If these areas are addressed, the time to recovery and recurrence rates can be greatly decreased. Footwear and training program analysis should also be performed to make sure they are tailored to your specific needs. It is recommended that you do not increase mileage by more then 10% per week in order to decrease the likelihood of developing MTSS.
The treatment options for ECS are similar to those for MTSS since poor running mechanics, improper footwear, and tight muscles can predispose you to being susceptible to this type of injury. More specifically, performing ART®, Graston, Medical Acupuncture, and other soft tissue techniques over the Tibialis Anterior, Calf Muscles, foot and toe extensors as well as the compartment fascia can help lower the pressure in the compartment and therefore decrease the pain associated with it.
Considerations
Two serious conditions can also be associated with common “Shin Splints”. The first results if a MTSS goes untreated for a long time and the activity is not modified appropriately. Then there is a chance of developing a tibial stress reaction. This Stress Reaction can lead to a visible stress fracture on X-ray which, if present, requires about 6-8 weeks of restricted physical activity and significant rehabilitation.

A more severe condition that may develop is called an Acute Anterior Compartment syndrome. This is a medical emergency since the pressure in the compartment can go so high that it cuts off blood and nerve supply to the muscles, ligaments, and bones in the lower leg and foot. The treatment is a surgical procedure called a fasciotomy. A fasciotomy involves cutting open a 4-6 inch section of the anterior compartment to decrease the pressure. Symptoms of this condition are extreme pain, swelling, numbness and lack of muscle control in the foot. These symptoms are similar to those of ECS except they are more intense and DO NOT decrease in intensity - they only INCREASE with time!
Summary
If you currently experience any of these symptoms, you should see a qualified health care practitioner to examine and evaluate your specific condition.
Disclaimer
This information is not intended to be a substitute for professional medical advice. You should not use this information to diagnose or treat a health problem or disease without consulting with a qualified health care provider. Please consult your health care provider with any questions or concerns you may have regarding your condition. Any attempt to diagnose and treat an illness using the information in this site should come under the direction of a trained medical practitioner. We accept no responsibility for any adverse effects or consequences resulting from the use of any of the suggestions or procedures in this site or related internet links. By using the information in this web site you are confirming that you understand this statement and that you accept all risk and responsibility.
All matters regarding your health should be supervised by your health care provider. All information provided in this site is for the purpose of education, not diagnosis or treatment.